- Approximately 75 - 80% of sleep apnoea people affected by sleep apnoea are not diagnosed with the disease because they have not been examined1
- If left untreated, sleep apnoea reduces life expectancy by up to 10 years2
- Untreated sleep apnoea significantly increases the risk of heart attack, heart failure, stroke, type 2 diabetes and high blood pressure
- The breathing disorder is easy to diagnose and highly treatable
Sleep apnoea’s harmful potential in terms of cardiovascular risks is mainly due to the fact that it is often left untreated. This is due to the fact that too few people go to the doctor because of breathing pauses during sleep, snoring and daytime sleepiness. You should take these warning signs in yourself or your relatives very seriously. This is because the disease and its consequences – the symptoms of sleep apnoea syndrome – can be very well treated, especially if the OSA is detected at an early stage.
If you also experience symptoms such as daytime sleepiness, or are prone to microsleep and rapid exhaustion, you should visit a sleep laboratory to diagnose possible sleep apnoea. Especially if your partner also tells you about nocturnal breathing pauses and loud snoring.
What are the different forms of sleep apnoea?
Obstructive and central sleep apnoea
Today, it is certain that moderate to severe sleep apnoea can lead to serious secondary diseases if left untreated. In the meantime, obstructive sleep apnoea (OSA) in particular has long since become a widespread disease. Often shortened to sleep apnoea, obstructive sleep apnoea is by far the more common form of sleep apnoea.3 It accounts for more than 90% of all sleep apnoea cases. The development of OSA into a widespread disease is related to the rapid increase in civilisation phenomena such as obesity, type 2 diabetes and stress.
But you should know that there is another variant of nocturnal breathing pauses: central sleep apnoea. This accounts for about 5% of all cases and is thus much rarer. In central sleep apnoea, a disorder in the central nervous system causes the breathing muscles of the chest and diaphragm to not work properly. The symptoms are similar: The focus is on repeated awakenings due to respiratory arrest, often accompanied by shortness of breath. The consequences here are also non-restorative sleep, insomnia and daytime sleepiness.4
However, the two forms of sleep apnoea differ significantly in their cause: While OSA causes a ‘collapse’ or closure of the upper airways, central sleep apnoea is caused by disturbances in the activation of all muscle groups required for breathing. This means that the brain ‘forgets’ to breathe evenly. Here, the recommendations for treatment as well as the symptoms that occur strongly depend on the underlying disease of central sleep apnoea. It can be the result of neurological diseases, opiod therapy, Cheyene-Stokes respiration or a stroke, for example. However, it can also occur temporarily at high altitude.4
Obstructive sleep apnoea can have serious health consequences and significantly worsen the quality of life of those affected and also that of their relatives, especially their bed partners. But only if it is not treated.
Listen carefully!
Compare breathing pauses with ordinary snoring now
Only 10% of all sleep apnoea patients are diagnosed. The main reason for this is that the dangerous breathing pauses are often mistaken for normal snoring sounds.
But you can clearly hear the difference. If you or your bed partner suffers from breathing problems, you should act now!

- Two different forms: Obstructive and Central. The common feature are repeated pauses in breathing during sleep. The treatment, however, is different.
- Obstructive sleep apnoea (OSA) is the most common form. In this case, the upper airways close again and again for a short time. The critical narrowing occurs due to slackening of the tongue muscle and adjacent areas.
- Central sleep apnoea (CSA) is due to a disorder in the central nervous system (CNS) that causes the breathing muscles of the chest and diaphragm to not work properly.
- Very rarely, mixed forms of obstructive and central sleep apnoea occur.
- The term sleep-related breathing disorder (SBAS) summarises a number of clinical pictures which are characterised by the occurrence of apnoeas and hypopnoeas. Central and obstructive sleep apnoea are also included, as well as Cheyne-Stokes Respiration (CSA). In this disease, shallow and deep breaths alternate during sleep, interrupted by central pauses in breathing.
What happens with obstructive sleep apnoea?
Obstructive sleep apnoea is one of the most underestimated widespread diseases, affecting around 20 million people in Germany, yet it is hardly known.5From the age of 60, around one in three men and one in four to five women are affected by sleep apnoea. The main risk factors for nocturnal upper airway collapse are advanced age and obesity. Loud snoring as a typical OSA symptom is often mistakenly dismissed as harmless, and so early detection of this serious disease is often delayed.
Over 95% of those affected in Germany are not diagnosed or treated5
The dangerous thing about obstructive sleep apnoea are repeated pauses in breathing during sleep, because the upper airways are unstable and sometimes close completely. If the airways close completely, the sleeper is cut off from the oxygen supply for a short time each time (apnoea). Airway obstruction leads to oxygen desaturation of the blood, causing an arousal reaction that often lasts only milliseconds but reopens the airway, preventing death by asphyxiation. This is favoured by anatomical risk factors such as a far-back lower jaw, enlarged tonsils, adenoids or a large tongue. Slipping of the tongue back into the throat can also lead to critical narrowing of the upper airway. But even if the airways are not completely blocked, the oxygen supply is still reduced to a critical extent (hypopnoea).
Repeated breathing pauses during sleep
Again and again, the breath stops at night because the upper airways close up, until they are completely blocked. The reasons for this vary from case to case. This happens by releasing stress hormones that increase heart rate and blood pressure. This is to provide enough nutrients for the muscles and organs to reactivate the respiratory muscles. And this sometimes happens dozens of times a night. Life-saving, but in the long run enormously stressful for the body and a great risk for the cardiovascular system.
„The breathing stops put the body under stress. You don't wake up consciously, but the restful sleep phases are disturbed,“ says Dr Hohenhorst, Alfried Krupp Hospital, Essen.
Hundreds of such incidents can occur per night in severe forms of obstructive sleep apnoea. But even mild forms of sleep apnoea are not trivial and should be taken seriously. On the other hand, not every cessation of breathing during sleep is the same as sleep apnoea. Even in healthy people, it sometimes happens that the airways narrow. As long as this does not happen more than five times within an hour, this is within acceptable limits.
At a glance: Breathing pauses during sleep
- Obstructive sleep apnoea is a condition in which breathing stops repeatedly during sleep, interrupting the flow of breath completely (apnoea) or partially (hypopnoea). The apnoea-hypopnoea index (AHI) is the measure of the severity of the condition.
- Even healthy people experience breathing pauses during sleep from time to time. Mild forms of OSA start from five breathing pauses per hour. In very severe cases there can be hundreds of breathing pauses per night.
- Why some people experience frequent breathing pauses during sleep has not been explained in detail. We know that different factors can contribute to the upper airways becoming blocked during sleep. The factors and other possible causes should be investigated in an individual examination, as these will guide the subsequent treatment.
For snoring, daytime sleepiness and breathing stops, off to the sleep lab

Find out about sleep apnoea diagnosis now
Many people who are affected by obstructive sleep apnoea don't even know about it. Most of them are probably aware that they snore, but they think nothing of it. Snoring is widespread, and in fact it is often simply an annoying phenomenon, but quite harmless. With sleep apnoea, however, it is different. In this case, snoring is an alarm sign. And if you experience daytime sleepiness - alone or in combination with snoring - you should also think about the possibility of obstructive sleep apnoea.
- Loud snoring (most of the time)
- Daytime sleepiness (almost always)
- Breathing stops – often combined with sudden waking and gasping for air, possibly with palpitations and shortness of breath. Most people affected by sleep apnoea do not notice the breathing pauses and the subsequent wake-up reaction.
- Restless sleep, sleep disorders
- Night sweats
- Headache in the morning
- Lack of concentration
- Memory problems
- Drop in performance
- Depressive moods (more common in women)
- Increased urination at night
- Erectile dysfunction or libido disorders
Partners of sleep apnoea sufferers often notice that the person withdraws, which can quickly affect their relationship. Those affected are quickly exhausted. Hobbies, friends and everyday tasks are neglected. This is because people with sleep apnoea experience symptoms during the day such as rapid exhaustion from everyday tasks, daytime fatigue, memory problems, poor concentration and mood swings. This occurs without an obvious cause, because they seem to sleep enough. They often wonder why they are constantly tired despite apparently(!) enough sleep.
At the same time, the sleep of the bed partner also suffers from the sleep apnoea symptoms. Either the loud snoring keeps them awake or the frightening silence during the breathing pauses.
An examination in the sleep laboratory should be carried out in any case. If, for no apparent reason, a person suffers from constant fatigue, lets friends and hobbies slide and withdraws, while at the same time their partners notice loud snoring and breathing pauses in their sleep, then they may have obstructive sleep apnoea.
So if you are constantly tired despite sleeping, and your bed partner frequently tells you about loud snoring and breathing stops, then these things may be related. Obstructive sleep apnoea could be behind the symptoms. In order to avoid serious secondary diseases of sleep apnoea, you should go to a sleep laboratory for diagnosis. Sometimes hypertension, i.e. high blood pressure, is also mentioned as a symptom of sleep apnoea. However, this is not quite correct, had high blood pressure is not a symptom, but a possible consequence of untreated sleep apnoea. So if you have been suffering from high blood pressure for a long time that does not respond to the usual antihypertensive drugs, it could be because the underlying OSA actually needs to be treated.
Daytime sleepiness despite several hours of sleep
Any cessation of breathing that occurs during sleep triggers a wake-up response in the brain. However, the sleeper does not fully wake up, but falls asleep again immediately after taking a deep breath. Most of the time the sleeper doesn’t even notice the incidents. It is not until the next morning that those affected realise that something is wrong: Although they have slept for hours, they do not feel refreshed. They wake up feeling tired and are tired all day long. They cannot concentrate and there can be dramatic drops in performance. People with severe forms of sleep apnoea feel so listless that they find the simplest everyday activities difficult.
Oxygen deficiency and disturbed sleep architecture
Daytime sleepiness has two causes: inadequate oxygen supply and disturbed sleep architecture. Our brain, which has to carry out highly complex tasks every day, reacts particularly sensitively if it is not properly supplied with oxygen. It is therefore no wonder that drowsiness, lack of concentration and other performance losses are consequences of repeated nocturnal breathing stops.
In addition, sleep must have a certain structure - the sleep architecture - in order to be restful. Healthy sleep consists of different phases: Sometimes we only sleep lightly, then again deeply and soundly. The REM phases (Rapid Eye Movement) have a special significance. In these sleep phases, the eyes move back and forth behind the closed eyelids at lightning speed: We dream and process our experiences. If the sleep architecture is disturbed, sleep loses its recreational value. So sleep duration alone is not decisive. If the sleep architecture is not right, you do not feel rested, despite sufficient sleep.
Those affected by sleep apnoea often nod off spontaneously during the day and some have experienced the shock of falling asleep at the wheel for seconds. The risk of accidents on the road has been shown to be increased with obstructive sleep apnoea.6 A scare caused by microsleep can be the ‘wake-up call’ that prompts people with obstructive airway disease to finally see a doctor. Unfortunately, many people affected delay this step for a long time. As daytime sleepiness is a rather unspecific symptom that can have many causes, very few people think that they may have a serious illness.
At a glance: OSA main symptom daytime sleepiness
Pauses in breathing reduce the blood oxygen content, impairing oxygen supply
Each breathing stop triggers an arousal response, disturbing a healthy, restful sleep architecture
Impaired oxygen delivery and disturbed sleep architecture are responsible for daytime sleepiness, a typical symptom of OSA
Daytime sleepiness is associated with reduced performance and an increased risk of accidents
Loud snoring is suspicious
Snoring is the second most important leading symptom of obstructive sleep apnoea, after daytime sleepiness. Most, but not all, people with OSA snore loudly. Many snorers have unsuccessfully tried a variety of home remedies to stop the annoying noise. It is largely unknown that snoring can be caused by a serious medical condition. Often, it is the frustrated sleeping partner who finally urges the snorer to see a doctor.
The combination of snoring and daytime sleepiness is also a strong indicator for obstructive sleep apnoea. Chronic daytime sleepiness occurs in almost all but the most mildly affected people and should be reason enough to get to the bottom of the problem. Snoring, on the other hand, may be absent. Some people with sleep apnoea do not make any sound when they stop breathing at night, making the condition even harder to detect.
Snoring is always a sign that the upper airways are unstable during sleep. In many cases, this is harmless, apart from the strain this puts on the partner. However, in the case of obstructive sleep apnoea, snoring is an alarm signal.
When should snoring be taken seriously?
But how can a layperson tell if their snoring is just a nuisance or a sign of a medical condition that needs treatment? Snoring that is loud and/or irregular is particularly suspicious. The best thing to do is to ask your sleeping partner, who may have noticed that you startle or gasp for air from time to time during your sleep. If so, this is red alert and you should see your doctor as soon as possible.
The combination of snoring and daytime sleepiness is also a strong indicator of obstructive sleep apnoea. Chronic daytime sleepiness affects - apart from the very mild cases - almost all people with OSA and should be reason alone to get to the bottom of things. Snoring, on the other hand, can also be absent. Some people affected by sleep apnoea do not make a sound when they stop breathing at night. Then it is even more difficult to detect the disease.
What are the causes and risk factors for sleep apnoea?
The causes of obstructive sleep apnoea are diverse and need to be assessed individually. A major cause of OSA is slackening of the muscles during sleep. In some people, the reduced tension state can lead to upper airway instability and collapse. The tongue muscle also plays an important role. When it is slack, it can slip into the throat and block access to the windpipe. Those affected can no longer breathe, causing the well-known breathing pause. Numerous risk factors and anatomical constrictions in the mouth and throat area favour the closure of the upper airways.
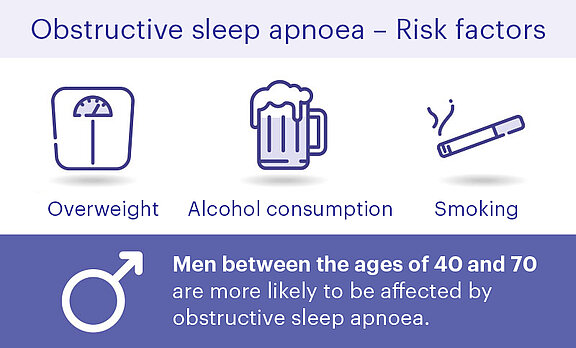
One of the biggest risk factors for obstructive sleep apnoea is being overweight. The excess pounds are not only located in visible ‘problem zones’ such as the abdomen and hips; overweight people also have more or less pronounced fat deposits inside the body. Fat deposits around the palate and throat can contribute to narrowing of the upper airways. If the muscles relax during sleep, obesity can make it even easier for the airways to close. Being overweight is therefore an important risk factor. More than 80% of people with obstructive sleep apnoea carry too many pounds.7
‘With every year of life, the risk of suffering from sleep apnoea becomes greater, just as the risk increases with every kilo,’ says Dr Hohenhorst, Alfried Krupp Hospital, Essen
The risk of obstructive sleep apnoea is also strikingly high in diabetics. Especially people with type 2 diabetes are affected, probably because most type 2 diabetics are ‘too fat’. Around 60% of all type 2 diabetics are estimated to be affected by obstructive sleep apnoea.8
Other lifestyle factors that promote OSA are: High alcohol and nicotine consumption, stress and the use of sleeping pills or drugs.
Another risk factor is age, because with increasing age, the risk of muscle-related instability of the upper airways increases and thus the risk of developing sleep apnoea. But gender also plays a role. In men, the number of cases rises steadily with age. In women, the risk of OSA increases significantly with menopause. Anatomical risk factors include enlarged tonsils, a short lower jaw, a crooked nasal septum or a too very tongue.


Sleeping on your back further promotes the closure of the airways. The possible anatomical peculiarities of the head and neck mean that the intraluminal suction during inhalation and the corresponding tissue pressure have a constricting effect on the volume of the upper airways.
Sleep apnoea causes & risk factors at a glance
- High body mass index (BMI 35 and higher)9
- Accompanying this: Fat deposits in the palate and throat area
- Advanced age10(one in three people aged 60 and over are estimated to have OSA): The entire musculature, and consequently also the muscles of the upper respiratory tract, loses tension with each year of life, which promotes airway obstruction
- Male gender
- For women, the risk increases during the menopause
- Type 2 diabetes - about 60% of diabetics also suffer from obstructive sleep apnoea8
Anatomical risk factors of obstructive sleep apnoea:
- Narrowing of the upper facial bones or upper airway
- Obstruction of airflow due to small lower jaw
- Enlarged tongue, adenoids or tonsils
- Crooked nasal septum
Lifestyles that promote obstructive sleep apnoea:
- Regular alcohol consumption, especially in the evening11, use of drugs or sleeping pills
- Heavy smoking11
- High levels of stress
- Unhealthy sleep hygiene
- Sleeping on your back
Sleep apnoea in men and women
In women, obstructive sleep apnoea often progresses silently without snoring sounds. This is one of the reasons why the disease is particularly often overlooked in women. Even the doctors who described obstructive sleep apnoea as a "new disease" about 40 years ago initially only had men in their sight. It was only much later that it was realised that women were also affected. The fact that women snore less often can be explained by anatomical differences in the throat area.
Up until the menopause, women are significantly less often affected by obstructive sleep apnoea than men. However, this is by no means a ‘man’s disease’, because after the menopause, the risk of disease increases sharply in women. This is probably mainly due to the fact that women often gain weight at this age. In men, on the other hand, the number of cases rises steadily with age.
More than a small difference
The symptoms of obstructive sleep apnoea also show gender-specific differences:12,13 As mentioned, women snore less often. Unlike men, women affected by sleep apnoea often consult a doctor because they suffer from problems falling and staying asleep. Women seem to be more sensitive to the nocturnal breathing pauses and wake up more often from them. Women also talk about depressive moods much more often. These are frequently at the top of the list of the complaints that women with sleep apnoea report when they visit their doctor. And a further difference was noticed in studies: Women with OSA experience restless leg syndrome more often than men. This is an agonising urge to move the legs that occurs mainly at night and makes it impossible to keep their legs still.
Sleep apnoea syndrome – secondary diseases and accompanying symptoms
Obstructive sleep apnoea is not trivial
Obstructive sleep apnoea is a serious condition and sleep disorder. This is true for adults as well as for children. There is a risk of health damage if the disease is not recognised and adequately treated. The quality of life is considerably reduced by the chronic daytime sleepiness and the loss of performance alone.
Sleep apnoea has many sequelae and accompanying symptoms
But that is not all: Obstructive sleep apnoea carries with it a number of secondary diseases, including various cardiovascular complications such as heart failure, high blood pressure, but also stroke and heart attack, as well as type 2 diabetes and depression. This is not surprising: The nocturnal breathing pauses are pure stress for the body, which can seriously upset the hormonal balance. The secondary diseases and accompanying symptoms such as daytime sleepiness, lack of concentration, memory lapses, erectile dysfunction and headaches are referred to as sleep apnoea syndrome. This syndrome has an enormous impact not only on the quality of life but also on life expectancy.6 If left untreated, sleep apnoea can reduce life expectancy by several years.2
'Many sleep apnoea patients are treated for high blood pressure over a long period of time when the underlying cause, the sleep apnoea itself, should have been treated first.' Dr Hohenhorst, Alfried Krupp Hospital Essen
If left untreated, obstructive sleep apnoea can lead to serious complications:
- Depression
- High blood pressure, often poorly treatable
- Heart attack
- Stroke
- Cardiac arrhythmias
- Type 2 diabetes
- Daytime sleepiness
Suspected sleep apnoea – When should you see a doctor?
If you snore loudly and/or are constantly tired during the day, you should have a check-up as soon as possible to see if you have obstructive sleep apnoea. Your doctor will proceed step by step to confirm or reject the suspected diagnosis. The targeted questioning (anamnesis) alone is very informative, which may be carried out with the help of standardised diagnostic questionnaires. It is best if your partner accompanies you to the doctor's appointment, as he/she can often provide important information.
Obstructive sleep apnoea is treatable
For moderate to severe obstructive sleep apnoea, positive pressure ventilation with a CPAP (Continuous Positive Airway Pressure) mask is currently recommended as the standard therapy. The patient has to wear a face mask while sleeping and is supplied with slightly pressurised breathing air via a tube from a device next to the bed. This treatment is able to effectively reduce nocturnal breathing pauses and reduce daytime sleepiness. But for many, CPAP therapy is not acceptable, as they feel constricted by the mask or suffer from side effects such as pressure sores and dry mouth. Therapy discontinuations therefore occur frequently.
In contrast, the satisfaction of patients who are fitted with an upper airway stimulation device is very high. According to surveys, over 90% would choose this form of therapy again.14 The upper airway stimulation device is implanted under the collarbone and ensures that the upper airways do not block at night. It continuously stimulates the tongue muscle and prevents it from slackening and slipping backwards. The breathing stops typical of OSA are thus avoided. As a result, daytime sleepiness decreases and performance improves.14 Inspire therapy offers an effective alternative for patients who fail CPAP therapy and other treatment options. With this innovative form of therapy, nocturnal breathing pauses are significantly reduced – without the need for a respiratory mask. The treatment is recommended as a therapy by the German Society for Sleep Medicine and Sleep Research for certain people for whom a CPAP mask does not have sufficient effect.15 The effectiveness of the upper airway stimulation device has been confirmed in various studies.14,16,17,18
How upper airway stimulation works for sleep apnoea
Discover Inspire therapy

Patient satisfaction14
Silent and simple use
Effectiveness17
Significantly reduces breathing pauses
At the touch of a button
Switch on at bedtime
No mask
has a lasting effect without annoying CPAP mask
References
1 www.lungenaerzte-im-netz.de/krankheiten/schlafstoerungen/prognose-verlauf/ - Zuletzt aufgerufen: Oktober 2020.
2 Muza, R.T., Central sleep apnoea-a clinical review. J Thorac Dis, 2015. 7(5): p. 930-7.
3 Hollandt JH, Mahlerwein M. Nasal breathing and continuous positive airway pressure (CPAP) in patients with obstructive sleep apnea (OSA). Sleep Breath. 2003 Jun;7(2):87-94. doi: 10.1007/s11325-003-0087-7. PMID: 12861488.
4 Deutscher Berufsverband der Hals-Nasen-Ohrenärzte e.V. Online verfügbar unter: www.hno-aerzte-im-netz.de/krankheiten/schnarchen-schlafapnoe/definition-und-haeufigkeit.html; Zuletzt abgerufen: April 2020.
5 Heinzer R. et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015 Apr;3(4):310-8. doi: 10.1016/S2213-2600(15)00043-0.
6 Deacon, N.L., et al., Treatment of Obstructive Sleep Apnea. Prospects for Personalized Combined Modality Therapy. Ann Am Thorac Soc, 2016. 13(1): p. 101-8.
7 Ancoli-Israel, S., Sleep apnea in older adults–is it real and should age be the determining factor in the treatment decision matrix? Sleep Med Rev, 2007. 11(2): p. 83-5.
8 Wetter, D.W. and T.B. Young, The relation between cigarette smoking and sleep disturbance. Prev Med, 1994. 23(3): p. 328-34.
9 Deutsche Gesellschaft für Schlafforschung und Schlafmedizin. Online verfügbar unter www.awmf.org/uploads/tx_szleitlinien/063-001l_S3_SBAS_2017-08_2.pdf - Zuletzt abgerufen: Mai 2020.
10 Deutsche Gesellschaft für Schlafforschung und Schlafmedizin (DGSM). Leitlinie S3 Nicht erholsamer Schlaf / Schlafstörungen. Kapitel „Schlafbezogene Atmungsstörungen bei Erwachsenen“.
11 Robert Koch-Institut. Gesundheitsberichterstattung des Bundes, Heft 27: Schlafstörungen. Online verfügbar unter: www.dgsm.de/downloads/fachinformationen/rki-bericht/schlafstoerung.pdf, Zuletzt abgerufen: Dezember 2020.
12 Valipour A et al. Gender-related Differences in Symptoms of Patients With Suspected Breathing Disorders in Sleep: A Clinical Population Study Using the Sleep Disorders Questionnaire. Sleep. 2007; 30(3):312-9. doi: 10.1093/sleep/30.3.312.
13 Mihai V et al. Demographic, Clinical and Polysomnographic Differences Between Men and Women.Pneumologia. 2010; 59(2):64-7.
14 Wiater A et al. Obstruktives Schlafapnoesyndrom im Kindesalter.Deutsches Ärzteblatt. 2002; 99(49): A-3324-30.
15 Acker J et al.: Obstructive sleep apnea (OSA) and clinical depression-prevalence in a sleep center. Sleep Breath. 2017; 21(2):311-18. doi: 10.1007/s11325-016-1411-3.
16 Heiser C et al. Post-approval upper airway stimulation predictors of treatment effectiveness in the ADHERE registry. Eur Respir J 2019;53(1):1801405.
17 Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG). Online verfügbar unter: www.gesundheitsinformation.de/behandlung-einer-obstruktiven-schlafapnoe.2120.de.html?part=behandlung-as - Zuletzt abgerufen: Mai 2020.


