CPAP problems: technical or therapeutic?
Depending on the difficulties encountered with CPAP therapy, people can contact their provider or their sleep doctor for problem solving. These can usually support people encountering difficulties with CPAP therapy quickly and effectively, and the therapy will soon show the desired success. But that is not always the case. Often, those affected then try to get further ideas and impulses in self-help groups in order to find a suitable solution.
Expert Tip: Document every improvement attempt you have made so far with provider and/or a medical professional (in the sleep lab):
- Where was the improvement attempt made (provider/medical practitioner/sleep lab)?
- What exactly was done?
- How often was the pressure readjusted?
- How many masks have you tried?
See a sleep doctor if you have therapeutic problems
If, on the other hand, there are therapeutic problems with a CPAP mask, a sleep doctor should be consulted. These include, above all, persistent daytime sleepiness because breathing pauses are not sufficiently reduced, as well as problems falling asleep and staying asleep.
Sometimes CPAP mask wearers suffer from shortness of breath or even panic attacks. In addition, there are frequent reports of too much pressure on the mask and too much air in the stomach, up to and including severe bloating. But too little air pressure can also lead to problems. Then nocturnal collapse of the airways continues.
In addition, a sleep doctor can also check whether there are other sleep disorders, such as insomnia or restless legs syndrome, which prevent CPAP therapy from being successful.
For many problems with CPAP therapy, providers and sleep labs can offer quick support and the therapy soon shows the desired success.
Unfortunately, this is not always the case. It is not uncommon for OSA patients to get caught in a ‘ping-pong game’ between sleep doctor and provider in search of a solution to their problems with CPAP therapy, whether technical or therapeutic in nature. Often, those affected try to get further ideas in self-help groups in order to finally find a suitable solution.
5 Steps from CPAP to Inspire therapy
If there is still no improvement after several attempts to find a solution together with the provider and the sleep laboratory or sleep physician, you can consider possible treatment alternatives such as Inspire therapy.
Step 1: Find out about Inspire
Upper airway stimulation works in harmony with the natural breathing rhythm and significantly reduces nocturnal breathing pauses – simply at the touch of a button. All information on how Inspire therapy works and how to use it can be found here, as well as the basic criteria.

To find out how positively Inspire can impact everyday life and quality of life, take a look at the testimonials of our Inspire users or join one of our webinars!
From now on, we will accompany you every step of the way on your personal path:
- from the identification of CPAP incompatibility or intolerance
- to referral to an Inspire specialist in your area,
- and throughout the four phases of treatment.
And even afterwards, when you have already arrived in your new everyday life with Inspire therapy, we will be happy to answer any questions, provide tips and background information.
Step 2: Find a treatment centre near you
If you are affected by sleep apnoea and are generally eligible for Inspire therapy, our Medical Support Team will help you find a specialised treatment centre near you and coordinate an appointment for an initial consultation at your local clinic or hospital. You can get an overview of the specialised centres in our doctor finder.
Step 3: Consultation at the treatment centre
During the initial consultation, the doctor in charge can get to know the person affected by sleep apnoea and his/her medical history. To do this, he or she looks through the available documents, which the patient ideally brings to the appointment. If the required documents are not available, the doctor can also request them. In addition, the ENT status is checked, which means the doctor will examine the throat.
Documents for the initial interview at the clinic:
- Own documentation of at least 2-3 unsuccessful improvement attempts with a doctor. The doctor can then transfer this information into the required PAP documentation.
- Current Polysomnography (PSG): Not older than two years and recording without (CPAP) therapy.
- Optional: a current polygraphy (PG)
- CPAP device or the SD card for readout
If no current, meaningful PSG or PG is available because the examination was too long ago or the patient's state of health has changed (e.g. weight gain, further illnesses and possibly new medication), this will be made up for on site. The appointment for this is then coordinated by the doctor or the clinic.
Step 4: Sleep endoscopy
To assess whether Inspire therapy is suitable for someone affected by sleep apnoea, a so-called sleep endoscopy (DISE) is performed. During a sleep endoscopy, patients are briefly put into a sleep-like state where the muscles of the upper respiratory tract slacken as in natural sleep. During the artificially induced sleep, the typical nocturnal symptoms affected by sleep apnoea then become apparent and the doctor can examine whether the patient’s anatomy is suitable for treatment with Inspire. The examination is usually done on an outpatient basis.
Step 5: Implantation, activation & aftercare
The upper airway stimulation device is implanted during a short inpatient stay. This requires only two small incisions on the neck and chest. After about two to four weeks, the surgical sites are completely healed.
As soon as the surgical sites have healed completely, the individual therapy adjustment and activation follow. After a familiarisation phase of about four weeks, the system is individually adapted to the patient’s needs in the sleep laboratory during an adjustment night and readjusted if necessary. Follow-up care takes place once a year with your treating sleep physician or ENT specialist. You can find more details about the treatment process here.
We will be happy to accompany you on your personal path from CPAP therapy to Inspire. For questions before and after the implantation of upper airway stimulation, we are always there for you – by phone, by email or via our social media channels.

90%
of bed partners report no or only light snoring.2

90%
of those affected say they are satisfied with Inspire therapy.3

79%
Reduction of nocturnal breathing pauses due to upper airway stimulation.2
80%
of those with an implanted system use it every night.2
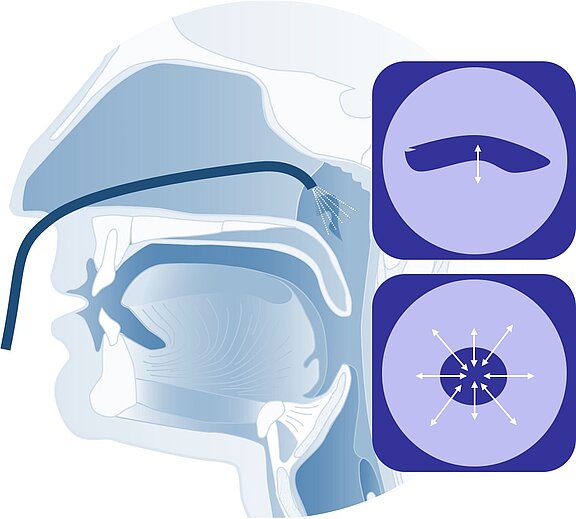
How Inspire therapy works
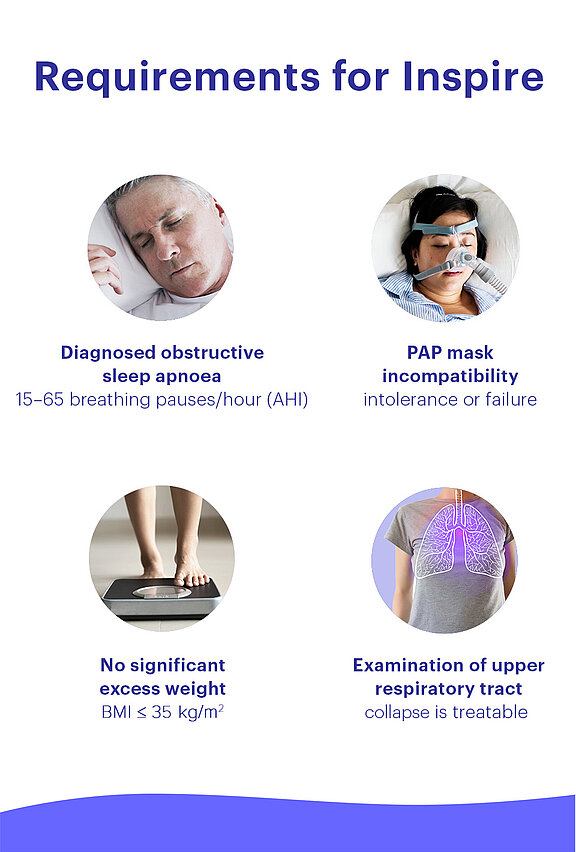
Thanks to the Inspire therapy, more than 60,000 patients worldwide can sleep through the night again. Inspire therapy is a fully implantable, proven effective and safe system for sufferers of obstructive sleep apnoea who cannot be treated or are not adequately treated with CPAP.
Upper airway stimulation works in harmony with your natural breathing rhythm and significantly reduces nocturnal breathing pauses – completely without a CPAP mask. With a remote control, the patient switches upper airway stimulation on at the touch of a button before going to bed and off again in the morning after waking up. The eligibility of those concerned is checked in medical examinations by a doctor. The procedure is performed in specialised treatment centres and clinics.
References
1 Bakker JP et al. Motivational Enhancement for Increasing Adherence to CPAP. Chest 2016;150(2):337-45. doi: 10.1016/j.chest.2016.03.019.
2 Woodson, BT, Strohl, K P, Soose, R J et al. Upper Airway Stimulation for Obstructive Sleep Apnea: 5-Year Outcomes. Otolaryngology–Head and Neck Surgery 2018; 159(1):194–202.
3 Heiser C, Steffen A, Boon M et al. Post-approval upper airway stimulation predictors of treatment effectiveness in the ADHERE registry. Eur Respir J 2019; 53(1):1801405.
The patient testimonials and sleep apnoea treatment reviews above relate to accounts of an individual’s response to treatment. The accounts are genuine, typical and documented. Responses to the treatment can and do vary. Not every response is the same. Patients received travel expenses and were compensated for their time in connection with this endorsement. Please review the safety information provided on this site and note that this therapy is not for everyone. Furthermore, the information on this site should not be used as a substitute for talking with your doctor. Always talk with your doctor about diagnosis and treatment information.






